Transiness Report (2026) Final ¦ 01/02/2026
Safeguarding Failures Affecting Transitioned Women
A Systems Analysis of Sexual and Domestic Violence Service Design
Why This Report Exists:
Quantifying the Failure of Services for Transitioned Women in England:
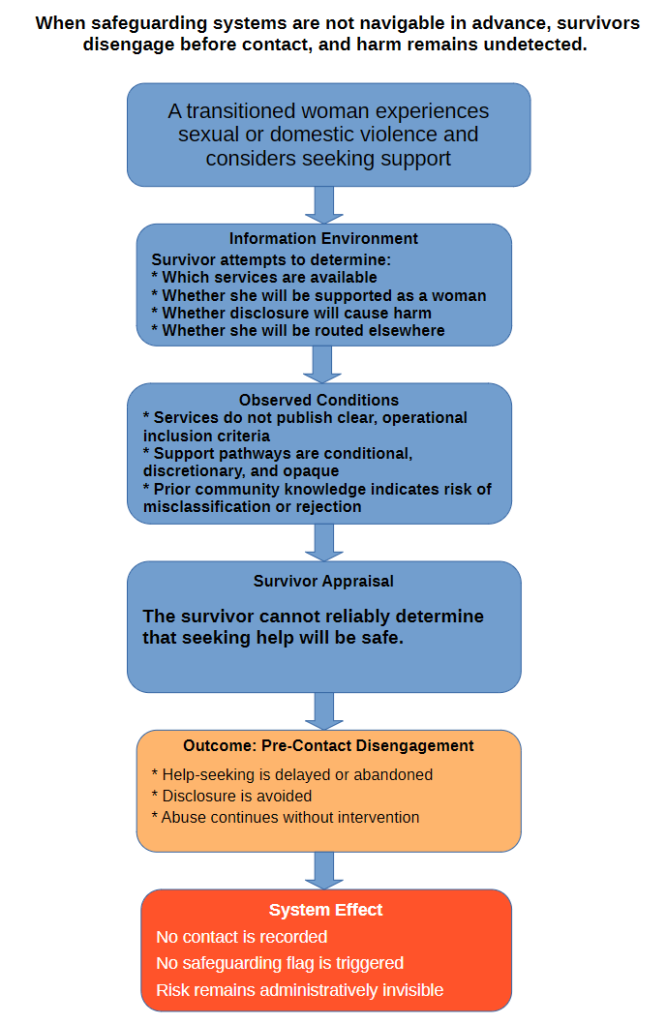
Safeguarding systems exist to respond to risk, not population proportion. When a group faces substantially elevated risk, as transitioned women do, services should scale accordingly. When they don’t, harm becomes not accidental but predictable and systemic.
For sexual violence specifically, a 2020 systematic review and meta-analysis estimates past-year sexual intimate partner violence (IPV) prevalence at 10.8% among transgender individuals, and finds that transgender individuals are 2.5 times more likely to experience sexual IPV than cisgender comparators within study populations.
Safeguarding systems exist to respond to risk, not raw population proportion. When a group faces markedly elevated exposure to harm, service provision must scale accordingly. Where this does not occur, exclusion becomes not accidental, but predictable and systemic.
Available evidence consistently demonstrates that transgender people experience substantially elevated rates of sexual violence relative to the general population. Community-based transition data further indicate that approximately 97% of trans people living in role have physically transitioned, are currently transitioning, or intend to transition. Of these, 45% have undergone both hormone therapy and surgery, 26% use hormone therapy alone, and 25% are actively awaiting treatment, with only 2.8% not seeking physical transition. This means that the overwhelming majority of trans women interact with support services as transitioned women, rather than as abstract identity categories.
Applying conservative UK population estimates (~0.2% of adult women) and established sexual violence prevalence ratios (4.1–4.5×), transitioned women should constitute approximately 0.8–0.9% of sexual violence service users per year within a fully functioning, non-exclusionary safeguarding system.
However, audit findings across England consistently demonstrate near-zero to <1% observed uptake, indicating that a substantial proportion of transitioned women survivors — typically between ~40% and 100% depending on locality — are failing to reach specialist support. In many regions, observed engagement approaches zero, indicating near-complete structural exclusion.
As of early 2026, only five sexual violence services in England provide clear, safe, navigable, and equivalent safeguarding pathways for transitioned women. The remainder operate frameworks in which exclusion is structurally embedded rather than episodic, resulting in the systematic non-delivery of safeguarding protection to a demonstrably high-risk population.
This is not a marginal gap. It is a system-level safeguarding failure, evidenced by:
- Near-absence from recorded service data
- Predictable disengagement after crisis contact
- Widespread healthcare avoidance
- Pathway collapse post-intervention
This briefing details why this failure occurs and what services can do to end it.
Abstract:
This report details systemic safeguarding failures in the UK affecting transitioned women who experience sexual or domestic violence. It identifies a critical service design mismatch where referral pathways prioritise administrative categories over the actual psychological and clinical needs of survivors.
The Core Problem
Sexual violence and domestic violence services exist because of specific expertise: understanding how abuse operates, how power imbalances function, and how institutional responses can either interrupt or compound harm. Yet in their response to transitioned women following the April 2025 Supreme Court ruling, many services are structurally reproducing the dynamics of abuse they exist to address.
Abuse operates through:
- Someone else is defining your reality
- Loss of agency and control
- Being told “this isn’t about you”
- Exclusion justified as “for the greater good”
- Being expected to endure harm quietly
When services treat the Supreme Court ruling as mandating categorical exclusion or birth-sex routing, they replicate these same dynamics at the institutional level:
- Reclassifying transitioned women against their lived experience and physical reality
- Forced categorisation without survivor consent
- Institutional responses are framed as “we have no choice” rather than active decisions
- Individual harm rationalised through appeal to collective safety
- Survivors required to accept therapeutic mismatch or categorical exclusion without complaint
This is not about individual practitioners’ intentions. It is about institutional design that mirrors the mechanisms of abuse itself. When services whose core expertise is recognising abuse dynamics implement policies that reproduce those dynamics at the institutional level, this represents a fundamental failure of safeguarding practice
Please download to read the full report.