When restriction is framed as care, and control is dressed up as safeguarding, it becomes harder to see the harm being done. This essay traces the logic behind gender-critical...
Leslie Feinburg's original intention behind it was honourable: it was to unite all people oppressed by cis-heteronormative gender constructs, people who do not neatly fit into the social...
People really love holding schemas about themselves and others, of gender and of embodiment (and a lot more), and make constructs which may feel right, or justified, or protective,...
By: Liora Wren (Transiness Admin) transinessadmin@protonmail.com Date: 5/10/25 Foreword: If this Sussex Police policy were framed so that cis women could be stripped and searched by men, the outrage...
When we first wrote to the Nursing and Midwifery Council (NMC) in February, we hoped for a response that would acknowledge the harm being done to trans patients and...
Recently, the UK Supreme Court delivered a decision that’s caused considerable anxiety among trans women across the country. Headlines shouted that we’ve been “banned” from women’s toilets, hospital wards,...
The Quiet Codification of Control: Trans People and the Infrastructure of Forced Visibility


6 min read
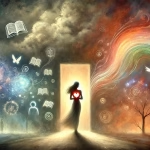
This week, the UK government confirmed what many of us feared: a centralised, non-consensual tracking system for transgender people is not only underway – it is being rationalised as...
In a world where people are taught what to feel and think about transitioned women, identifying good therapy is vital. So often you come across this phenomenon in therapy:...
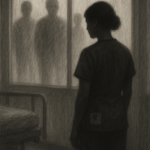
Introduction When we talk about medical chaperones, what are we really talking about? Officially, a chaperone is someone present during medical examinations, particularly intimate ones, to safeguard both patient...
The Nursing and Midwifery Council (NMC) is entrusted with upholding the integrity and professionalism of nursing and midwifery in the UK. Yet, recent events have exposed a disturbing trend:...